Rifaximin alters the intestinal microbiota to prevent inflammation and visceral hyperalgesia in stressed rats, according to the February issue of Gastroenterology. These findings could explain the ability of this antibiotic to relieve symptoms of irritable bowel syndrome (IBS) in patients.
Rifaximin is a broad-spectrum antibiotic that has been approved by the FDA for traveler’s diarrhea and minimal hepatic encephalopathy. Interestingly, rifaximin also appears to reduce pain and bloating in patients with IBS, but little is known about the mechanisms of this process.
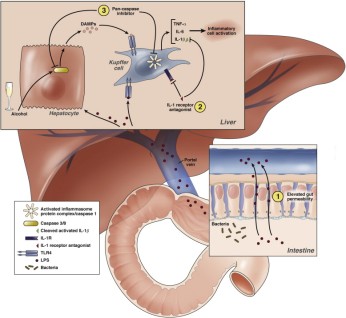
Low-grade mucosal inflammation and increased intestinal permeability are common in patients with functional bowel disorders. Chronic stress contributes to functional bowel disorders and can predispose patients to gastrointestinal infections or induce visceral hyperalgesia. In animal models of visceral hypersensitivity, psychological stress appears to alter gut microbiota and gut barrier function.
Xu et al. therefore used rat models of visceral hyperalgesia to determine how rifaximin affected intestinal microbiota, inflammation, and function. They found that induction of stress, by water avoidance or repeat restraint, led to visceral hyperalgesia, accompanied by mucosal inflammation and impaired mucosal barrier function.
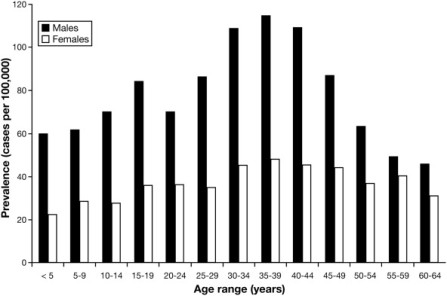
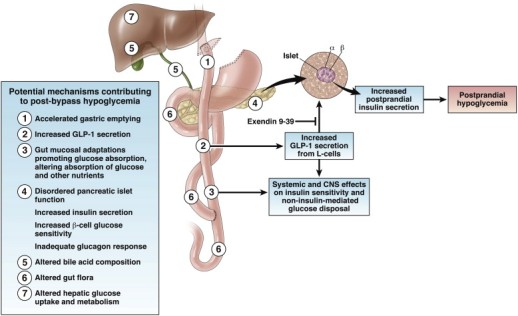
Oral administration of rifaximin reduced the bacterial load in the intestines of the stressed rats, and altered the composition of bacterial community in the distal ileum (Lactobacillus species became the most abundant, see figure.

Bacterial community composition analyzed with nonmetric multidimensional scaling plots using a θYC distance matrix of operational taxonomic unit−based data. Circles represent distinct bacterial communities identified in luminal contents of terminal ileum of individual rats. Circles that appear larger are closer in the axis not represented and circles that are smaller are farther away in the axis not represented; some circles have been made transparent.
Rifaximin also prevented mucosal inflammation, barrier impairment, and visceral hyperalgesia in response to chronic stress.
A different antibiotic, neomycin, also changed the composition of the ileal bacterial community (Proteobacteria became the most abundant species), but did not prevent intestinal inflammation or induction of visceral hyperalgesia by stress.
The authors propose that development of visceral hyperalgesia is likely, at least in part, mediated by specific interactions between the microbiota and mucosa that lead to inflammation and barrier impairments after exposure to chronic stress.
Preclinical and clinical studies have linked visceral hyperalgesia to increased intestinal permeability. Previous studies have shown that intestinal inflammation induced by chronic stress releases factors such as prostaglandin E2, and activates ion channels in the dorsal root ganglia that innervate the lower gut.
Psychological stressors have been reported to alter bacterial community structure. Studies have shown that the stress can change the bacterial community structure, reducing species richness and diversity, and facilitating susceptibility to bacterial pathogens.
Although rifaximin appears to alter intestinal bacterial communities, leading to a relative abundance of Lactobacillus that prevents mucosal abnormalities and visceral hyperalgesia induced by chronic stress, direct immunomodulatory effects might also be involved. However, the authors provide evidence that the effects of rifaximin observed are not caused by direct anti-inflammatory action on the mucosa.
Several clinical trials have evaluated the efficacy and safety of rifaximin in patients with IBS. A meta-analysis found rifaximin to be more effective than placebo in improving overall symptoms and bloating in IBS. Rifaximin has been estimated to offer an approximate 10% therapeutic gain for patients with IBS—similar to other available IBS therapies.
Xu et al. warn that rodent models have limited predictive value for IBS treatment in humans, and that the experimental design does not indicate that rifaximin treatment is beneficial for the symptomatic patient but rather that rifaximin prophylaxis can be beneficial in preventing a stress-induced flare.